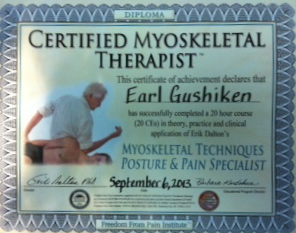
Studying and applying Erik Dalton “Motion with Lotion”
How Bodywork Lubricates Joints and Fascia
Is Motion ‘the’ Lotion
by Erik Dalton, Ph.D.
There’s a saying in orthopedics that “motion is lotion for joints,” but what about muscles, fascia, and neural structures? Aging causes us to produce less synovial fluid for joint lubrication, and hyaluronic acid for musculofascial gliding (Fig 1). Consequently, each day our bodies “dry up” a bit, get a little shorter, and hurt more. Living structures are perfectly adapted to work with maximal efficiency and low levels of energy. Sadly, our clients often present as noisy machines, which waste a lot of energy. But, motion is lotion and nothing brings back the juice like good bodywork and corrective exercise. The burning question is: “how does hands-on therapy produce the ‘lotion’ that restores ‘motion’ to stuck fascial layers, adhesive joint capsules, and injured ligaments”?
Some researchers believe that dried-up hyaluronic acid (HA) due to lack of movement, postural stress, or tissue injury, may be the glue that causes fascial adhesions. Hyaluronic Acid or hyaluronan is present in every tissue of the human body. It is most concentrated in the synovial fluid which bathes the joints, but also appears at the junction between the deep fascia and the muscle layers (Fig 2). In a fully functioning body, fascial layers secrete HA which allows smooth gliding between fascia and neighboring muscles. But, tissue trauma, overuse, and resultant inflammation can cause overproduction of HA, leading to molecular fragmentation and degradation. In time, the granulated particles form a sticky, dehydrated gel which may decrease fluidity, resulting in a binding or “gluing” of myoskeletal layers.
Most manual therapist’s hands have experienced the deep tissue release that comes when slow sustained pressure is applied to thickened fascia or fibrosed joint capsules. But, as yet, no one has presented clinical evidence for the histological changes that occur during this tissue remodeling. Dr. Philip Matteini, et al, found that HA molecules progressively broke down when the temperature was increased to 99-104º F.1 Although research is still limited, it is theorized that manual pressure may create a local inflammatory process and, as temperature increases, the dried-up hyaluronic gel rehydrates into a more fluid-like medium. This transformation may be what therapist’s feel as the tissue slowly yields to steady deliberate hand, elbow and finger pressure.
Whether the release we feel is from the ‘gel-to-sol’ hyaluronic acid transformation or a neural explanation such as fascial mechanoreceptors, practitioners must first hone their palpation skills to differentiate quality, range and end-feel of various soft tissues including joint capsules. Mentally ask yourself, during end-range of motion; does this tissue have a boggy, leathery, spasmodic, or hard end-feel? When comparing side-to-side, are there areas of bind in one limb and greater ease of movement in the other? What about hypermobility, length/strength imbalance, and resultant loss of proper joint centration?
In our new ‘Motion is Lotion’ 3-dvd set, my special guest Paul Kelly and I offer the following formula for restoration of pain-free movement:
• Recognize the restriction
• Restore mobility
• Rehab through movement
• Reintroduce the activity
Hopefully, the routines presented in my new videos (see video) will produce a number of beneficial effects for competing athletes, computer addicts, as well as our elderly population. The art of restoring pain-free range of motion and joint-play should rank high on today’s bodyworker’s list of treatment protocols.
1. Matteini P, Deil, Carretti E, Volpi N, et al. Structural behavior of highly concentrated hyaluronan. Biomacromoleculoes, 2009;10(6):1516-1522.
2. West DC, Shaw DM, Lorenz P, Adzick NS, Longaker MT. Fibrotic healing of adult and late gestation fetal wounds correlates with increased hyaluronidase activity and removal of hyaluronan. Int J Biochem Cell Biol, 1997;29:201-210.